Lumbar Stenosis
What is Lumbar Stenosis?
‘Stenosis’ is derived from a Greek word ‘Stenos’ which means to narrow.
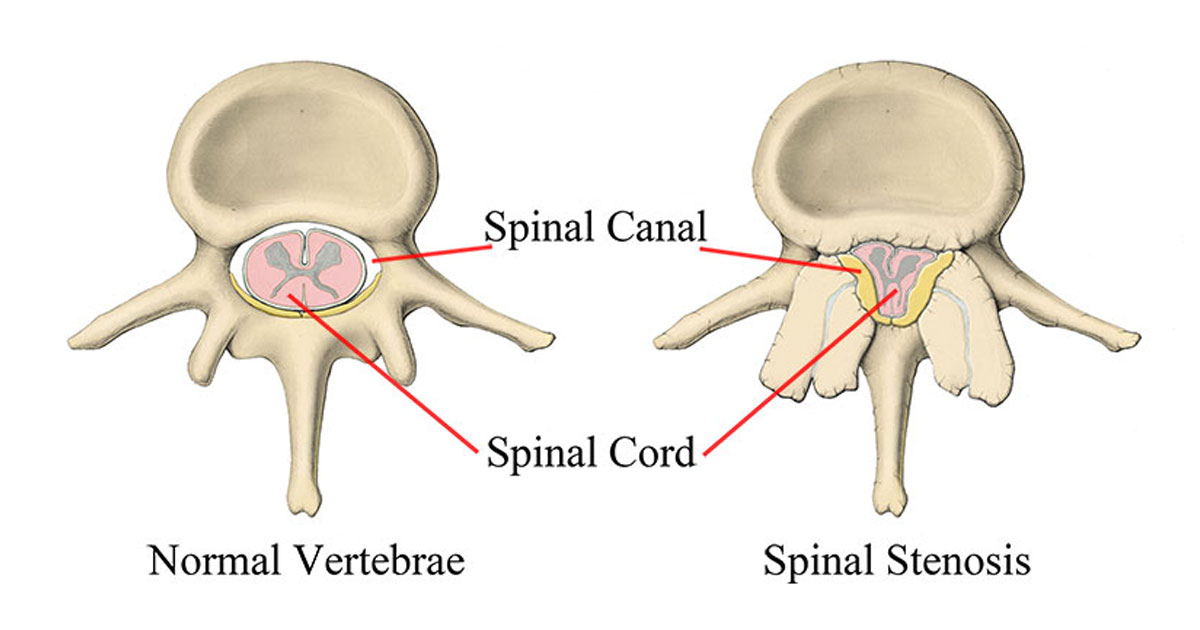
Therefore, stenosis essentially means narrowing. In the case of Lumbar Stenosis, this means that the central spinal canal, which is the canal at the centre of the spine, is becoming narrowed. The spinal cord and other important blood vessel structures are contained within this canal. Therefore, if stenosis is present it may cause insult to these structures, leading to neural and/or vascular symptoms. See the above image to get a basic visual idea of what happens to the spine with lumbar stenosis.
Figure 1 – Axial view (from above) of the Lumbar Spine, showing the difference between a normal and stenotic vertebra (backbone)
What causes Lumbar Stenosis?
Stenosis can be caused by genetic, acquired, vascular, or inflammatory factors, or a combination of these factors. Note that when someone has both genetic and acquired factors evident together simultaneously, this will significantly increase the risk of stenosis.
Genetic (Congenital) Factors
- Achondroplasia - the most commonly occurring bone growth disorder, occurring in approximately 1 in 20,000-30,000 people. This genetic disorder is caused by a change (mutation) in the fibroblast growth factor receptor 3 (FGFR3) gene.
- Short pedicles - when the pedicles (space between the spinous process and transverse process) of the vertebrae are shorter in length this can decrease canal size.
- Canal shape - People with a round canal have a low chance of stenosis, people with an ovoid-shaped canal have a moderate chance of stenosis and finally a person with a trefoil shaped canal has a higher chance of getting stenosis.

Figure 2 – Different Shapes of Central Spinal Canal
Acquired Factors
- Disc Bulge / Herniation – Stenosis can happen when a disc bulges outwards and moves into the central canal space.
- Facet Joint Hypertrophy/Bone Spurs – Stenosis can occur via hypertrophy (enlargement) of the facet joint or from developed spurs (bony growths) due to stresses placed on that joint.
- Thickened Ligamentum Flavum – Thickening of this ligament can cause stenosis
- Spondylosis/Spondylolisthesis – Stress fractures in the spine (Spondylolysis) or Slippage of one vertebra over another (spondylolisthesis) can also cause stenosis.

Figure 3 – Examples of some Acquired Factors Causing Stenosis
Vascular Factors
Stenosis can be caused by disease of the blood vessels within the body. Stenosis has been linked to 4 major blood vessel diseases, which are seen below.
Arteriosclerosis, Hypertension, Diabetes, Hyperlipidaemia
Arteriosclerosis is the build-up of fat and plaque in the arteries that causes the arteries to narrow. This is a condition that is shown to be linked with Lumbar Stenosis. Hypertension (high blood pressure), diabetes and hyperlipidaemia (high amount of fat in the blood) are also found to be linked with Lumbar Stenosis.
In a recent study in 2021 that examined the link between ‘chronic diseases’ (arteriosclerosis, diabetes, hypertension, hyperlipidaemia) in people over 50 years of age and lumbar stenosis, it showed that;
“Patients with Lumbar Stenosis and no chronic disease made up 35.2% (of the sample group), while the patients with chronic disease (one or more) made up 64.7%…
The patients with a single disease made up 29.5%... Patients with more than one chronic studied disease were 35.2%.” (Aitaha et al.)
To conclude this study, if you have all of these conditions your likelihood of obtaining stenosis almost doubles compared to someone without these diseases.

Inflammatory Factors
Inflammation can cause stenosis as a result of a process called the inflammatory cascade. Inflammation usually arises as a response to an acquired factor such as a disc or facet joint injury. The acquired injury stimulates an inflammatory response, which then can insult the nerve roots around the area causing swelling. This swelling triggers the release of inflammatory chemicals and leads to radicular pain (nerve pain).
Insult to disc/facet joint Inflammatory Response Insult to Nerve Roots Swelling Inflammatory Chemicals Stenosis Radicular Pain
How do you diagnose Lumbar Stenosis?
When diagnosing Lumbar Stenosis there are a few key signs to look out for to fit the clinical picture for this condition. Stenosis is more common in people aged 60 or older and in those who are overweight. Typically Stenosis will present with pain that has lasted for longer than 6 months and is interspersed with acute episodes of pain within that time period.
Patients with Stenosis will often not like prolonged extension-based activities such as standing or walking. Furthermore, flexion based activities will reduce pain. It is not uncommon that patients will experience altered sensation, cramping in the lower legs and may have reduced peripheral pulses and/or altered sensation in the feet. This is the case because of a phenomenon called claudication which can be vascular (relating to blood vessels) or neurogenic (relating to nerves).
Imaging can also be used to diagnose Lumbar Stenosis. The most common sign that indicates stenosis has occurred on a scan is called the ‘Nerve Root Sedimentation’ sign. It has an accuracy of 94% in identifying stenosis clinically.

Figure 4 – Visual Representation and MRI scan showing the Nerve Root Sedimentation Sign indicating Stenosis.
How do you treat Lumbar Stenosis?
In cases of stenosis that are not hereditary (genetic), Physiotherapy can be beneficial. Some methods of treating Lumbar Stenosis are listed below.
- Flexion Based Exercises – provides pain relief via opening the central canal and associated structures around the central canal. E.g. Child’s pose, knee hugs, knee rocks.

Figure 5 – Variations of the ‘Child’s Pose’ Stretch, used to open up the lower back.
Alter G Treadmill – At Spectrum Healthcare we have access to a state-of-the-art anti-gravity treadmill that allows the patient to walk normally with only a percentage of their body weight. This allows the patient to still be able to walk without pain, yet simultaneously allows there to be sufficient conditioning occurring.
Education – General education surrounding general lower back pain and stenosis, what to do and what not to do can be beneficial for all patients. Self-management, as well as injury prevention, is key!
Multifidus Strengthening – Multifidus is a muscle that runs along the whole length of the spine and is important in spinal stabilisation. Weakness and atrophy (shrinking) of the multifidus muscle is associated with low back pain. Research has shown that “The stenotic segments of the spinal canal are more atrophied than the non-stenotic segment in Lumbar Stenosis patients. It shows that there is a strong positive correlation between the severity of multifidus atrophy and the severity of spinal stenosis.” (Xia et al.)
Traction – Applying traction to the lumbar spine is a great way to alleviate pain and decompress the spine.
Lumbar rotation in side-lying – Put simply bringing your leg across your body with your affected side facing up can be another effective opening technique to achieve pain relief and decompression of the spine.
Increase Thoracic (Mid Back) and Hip Extension – By promoting increased movement at the adjacent areas to the lumbar spine it works to reduce the amount of stress on the lumbar spine. If you think of the spine and hips as two ends of an elastic band, and each end is pulled, this will make the middle of the band more taught. This same principle occurs here with the lumbar spine. By decreasing the tension at both ends there will be less tension in the middle of the band (lumbar spine).
Do you need surgery for Lumbar Stenosis?
Surgery, as for any injury should be a last resort. If all conservative measures have failed including physiotherapy, exercises, and corticosteroid/plasma injections, then surgery may be the best course of action for you.
When deciding whether to have surgery for lumbar stenosis the patient must take into account; the effect this injury is having on their everyday life, activities of daily living and mental health. Another element to be considered is the expected rehabilitation that will be required post-surgery.
According to research, for spinal stenosis “Surgery groups showed better late clinical outcomes after one year (compared to conservative treatment).” (Ma et al.)
A commonly performed surgery used to improve canal stenosis is called a laminectomy. In this surgery, the lamina of the vertebra is removed. This allows there to be a lot more room within the central canal, decompressing the spinal cord and vascular structures.

Figure 6 – Visual Representation of a Lumbar Laminectomy Procedure
References:
Aitaha, M. T., Saeed, M. A. M., Chasib, R. J., & Hamdan, T. A. (2021). Correlation between degenerative lumbar spinal stenosis and systemic diseases. Journal of Orthopaedics Trauma Surgery and Related Research, 16(7).
Ma, X., Zhao, X., Ma, J., Li, F., Wang, Y., & Lu, B. (2017). Effectiveness of surgery versus conservative treatment for lumbar spinal stenosis: A system review and meta-analysis of randomized controlled trials. International Journal Of Surgery, 44, 329-338. doi: 10.1016/j.ijsu.2017.07.032
Nerland, U., Jakola, A., Solheim, O., Weber, C., Rao, V., & Lonne, G. et al. (2015). Minimally invasive decompression versus open laminectomy for central stenosis of the lumbar spine: pragmatic comparative effectiveness study. BMJ, 350(apr01 1), h1603-h1603. doi: 10.1136/bmj.h1603
Piechota, M., Król, R., Elias, D., Wawrzynek, W., & Lekstan, A. (2018). The nerve root sedimentation sign in diagnosis of lumbar spinal stenosis. Acta Radiologica, 60(5), 634-642. doi: 10.1177/0284185118795322
Xia, G., Li, X., Shang, Y. et al. Correlation between severity of spinal stenosis and multifidus atrophy in degenerative lumbar spinal stenosis. BMC Musculoskeletal Disorders 22, 536 (2021). https://doi.org/10.1186/s12891-021-04411-5
