
Pelvic girdle pain in pregnancy
Up until the mid-90’s, pelvic girdle pain was long considered an extension of low back pain. It describes sharp, stabbing or aching pain anywhere between the bony prominences at the waist and the bottom of the glutes. Pain can sometimes refer down the back of the thigh and be accompanied by an uncomfortable grinding or clicking around the pelvis. It has only been in the past 20 or so years that health professionals have come to recognise that pelvic girdle pain is separate from low back pain, and as such, requires its own specific treatment.
Pelvic girdle is dissimilar to general low back pain as it is often more limiting in everyday life. Commonly our patients will report a reduced ability to keep standing, walking and sitting. Typically, pain is sudden and intense but eases quite fast with rest, lying down or support.

Who’s affected?
In the general population, pelvic girdle pain often accompanies low back pain. A study examining 100 people with low back pain found 13% of participants have intra-articular sacroiliac joint pain2, that is, pelvic girdle pain. However, the large majority of people who suffer from pelvic girdle pain will be women during pregnancy. Approximately 20-25% of pregnant women will experience pelvic girdle pain1, commonly starting in the 2nd and 3rd trimesters.
This number is so high in pregnancy for a couple of key reasons:
- Hormonal changes: during pregnancy there’s an increase in hormones, such as oestrogen and progesterone, which help to soften ligaments and increased joint mobility to prepare for childbirth.
- Increase in the load and stretch on the supportive tissues: as the body changes to accommodate a growing baby, there is both an increase in weight and stretch on the surrounding muscles and fascia, particularly the abdominal muscles and the pelvic floor.
- Changes in posture: as the baby sits at the front of our body the weight of the baby often shifts our bodyweight forward, leading to an increases the curve of the spine and a forward tilt of the pelvis. This isn’t necessarily a problem, but can reduce the mechanical advantage our muscles have and lead to earlier muscular fatigue.
What causes pelvic girdle pain?
Although there are many different factors affecting the pelvic girdle region during pregnancy, pelvic girdle pain in both populations (general and during pregnancy) is commonly deduced to the same thing:
Non-optimal stability of the pelvic girdle joints
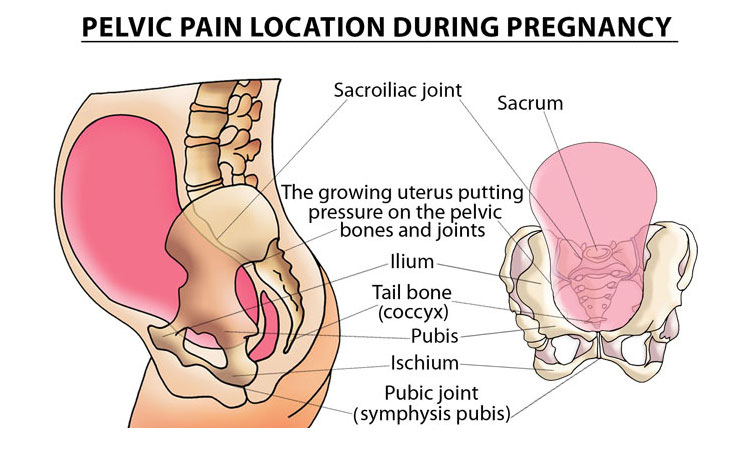
Specifically the pubic symphysis (at the front) and sacroiliac joints (at the back). Stability is the ability of our ligaments and muscles to alter joint laxity or stiffness to suit the task at hand – using the least amount of effort needed to prevent unwanted movement within the joints (not too little and not too much).

How is pelvic girdle pain treated?
Unfortunately we can’t change our bony structures, ligaments and hormones. However, because stability is also a function of muscular strength and coordination, pelvic girdle pain can be improved with targeted strengthening, even during pregnancy.
One thing to note is that in pelvic girdle pain treatment and exercise is not a “one size fits all”. As the pelvic girdle is quite a complex structure, a person can experience instability in a multitude of ways. Not everyone will need glute strengthening and not everyone will benefit from taping or bracing. The European Guidelines for pelvic girdle pain developed in 2007 recommend an individualised treatment and exercise program to match a person’s pattern of pain, which can be done by a Physio, Sports Chiro or Women’s Health Practitioner.

References
1. Vleeming, A., Albert, H. B., Ostgaard, H. C., Sturesson, B., & Stuge, B. (2008). European guidelines for the diagnosis and treatment of pelvic girdle pain. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society, 17(6), 794–819. doi:10.1007/s00586-008-0602-4
2. Schwarzer AC, Aprill CN, Bogduk N. The sacroiliac joint in chronic low back pain. Spine (Phila Pa 1976). 1995 Jan 1;20(1):31-7. PubMed PMID: 7709277.
